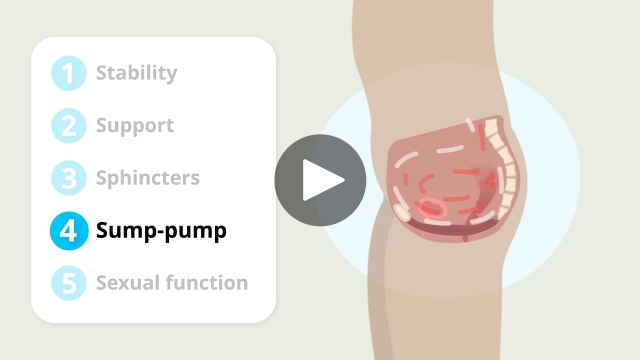
Understanding the pelvic floor
Learn about the pelvic floor, including basic pelvic floor care.
Common pelvic floor concerns
There are a number of activities and situations that can interfere with the natural movement of the pelvic floor and contribute to tightness in that area. This includes:
- Wearing chest binders or shapewear
- Shallow breathing, which can be caused by anxiety
- Having rounded posture
- Being injured or in pain
- Holding tension in the stomach, such as if you often suck in your belly
Wearing tight undergarments can irritate the pelvic floor, including the skin and organs, and contribute to any tightness in the pelvic floor.
Tucking Method of positioning the penis and testicles so as to conceal them. constricts blood flow, nerves, and ligaments, and restricts the movement of the pelvic floor region. If practiced regularly, this can contribute to pelvic floor tension over time.
Many people experience pelvic floor issues. While common, they don’t have to be your “normal.” These difficulties can often be managed and improved with treatment, including pelvic floor physiotherapy.
This refers to leaking urine, feces, or gas, with or without a strong urge to use the bathroom. It can affect anyone at any age. It can be caused by overactive pelvic floor muscles, injuries, stress, genital surgeries, gonadectomies, giving birth, holding in urine for long periods (e.g., when avoiding using shared or public bathrooms), incomplete emptying of the bladder (e.g., when rushing on the toilet), and certain medications.
Pelvic floor contraction exercises, also known as ‘“Kegels,” can sometimes worsen incontinence.
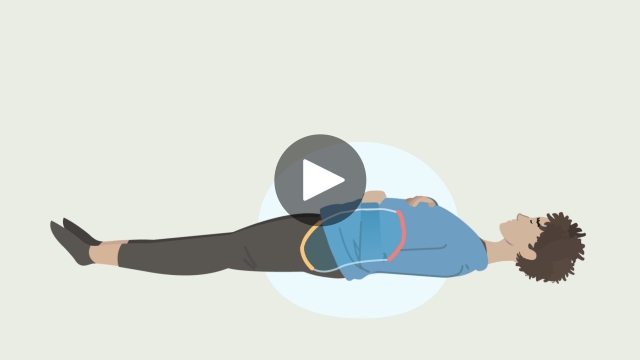
Diaphragmatic breathing is a safe activity that can be done at home to connect with the pelvic floor and start to address incontinence.
View our video on diaphragmatic breathing below.
Constipation can involve irregular bowel movements or straining.
"Regular" bowel movements can vary from once or twice a day to three times per week. The appearance of our bowel movements can also give us more information about our pelvic health. To learn more, check out the Bristol Stool Scale to help you understand what your bowel movements might indicate.
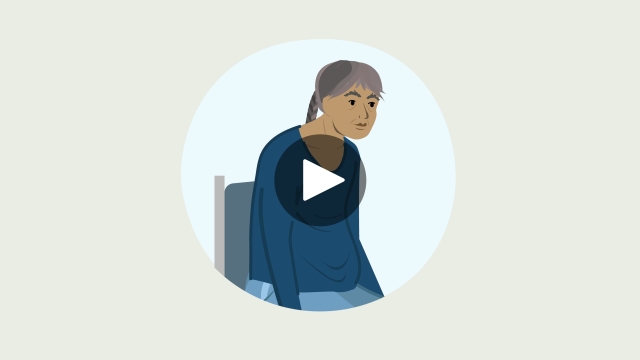
Speak with your primary care provider A person’s main health care provider in non-emergency situations such as check-ups and referrals. Family doctors, general practitioners (GPs) and nurse practitioners (NPs) are all primary care providers. if you are experiencing chronic constipation. Safe activities you can do at home to help ease constipation include:
- Using a small footstool to raise your knees above hip height. This position helps relax the pelvic floor, making bowel movements easier.
- Taking deep breaths instead of straining or trying to force out a bowel movement.
- Ensuring you are getting enough fiber and water in your diet.
- Getting some movement during the day.
Pelvic floor muscles play an important role in core stability. Tension or weakness in the pelvic floor and chronic constipation can both contribute to back pain.
Pain with insertion in the genital or rectal openings, such as with receptive sex, physical examinations, or menstrual products, is common but can often be eased with treatment. Kegels are often suggested as a way to treat these issues, but they can sometimes worsen symptoms. Instead, techniques that lengthen and release the muscles may be more effective.
Frequent bathroom trips and a sudden, intense urge to urinate (“0–100” urgency) are common bladder symptoms.
On average, people urinate five to eight (5–8) times per day, for around eight to ten (8–10) seconds of flow. However, this can vary based on hydration levels and what you have been drinking.
A helpful strategy is to avoid going to the bathroom “just in case”. Doing so can confuse the bladder and increase the sense of urgency. Try to only use the bathroom when you truly need to go.
If you experience frequent urination, staying well-hydrated and being mindful of bladder irritants can help. Common irritants include caffeine, alcohol, carbonated drinks, artificial sweeteners, citrus, chocolate, and spicy foods.
You do not need to eliminate these completely. For example, you could try drinking water before and after consuming them, or finding alternatives on occasion. Just being aware of how it impacts your body can help you make informed choices.
Pelvic health therapy
What is pelvic health therapy?
Pelvic health therapy is care provided by specially trained physiotherapists or occupational therapists. Not all physio or occupational therapists have training in this area, so it is important to find a provider who does.
The focus of pelvic health therapy is treating concerns related to the pelvic floor muscles using a personalized, whole-body approach. It combines hands-on care, guided movement, environmental and behavioral strategies, neuromuscular retraining, and more. It can be tailored to individuals of all ages, genders, life stages, and abilities.
A common misconception is that pelvic health therapy requires internal pelvic exams. While these can be useful, they are not necessary for effective treatment. Pelvic health providers are trained to discuss when a pelvic exam might be useful and tailor treatment plans to your needs and preferences.
Pelvic health care and surgeries
Pelvic floor therapy can be very helpful for surgeries, especially lower body surgery. Each person’s body is different, and pelvic floor therapists can screen for symptoms and provide tailored care plans both in preparation for, and after, your surgery.
How to get pelvic health care
Many people find gender-affirming providers through word-of-mouth. Another way to find a pelvic health therapist is to search the directory at the Pelvic Health Solutions website and filter for practitioners who have taken the course, “Introductory Pelvic Health Care for Trans and Gender Diverse Refers to gender roles and/or gender expression that do not match social and cultural expectations. People.”
Access can be limited, especially in rural areas or due to insurance coverage. If in-person visits are challenging, or if finding a gender-affirming provider nearby is difficult, virtual visits can be a valuable alternative. The exercises on this webpage are also a good starting point.
Basic pelvic floor care
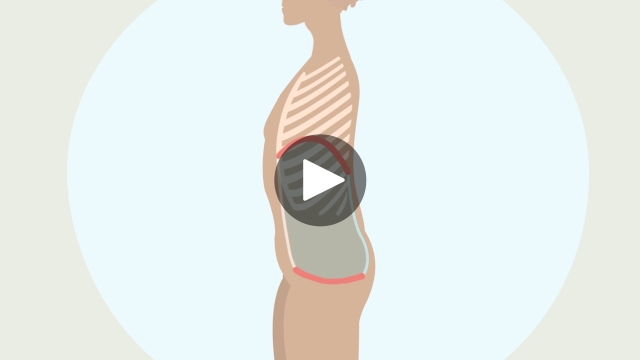
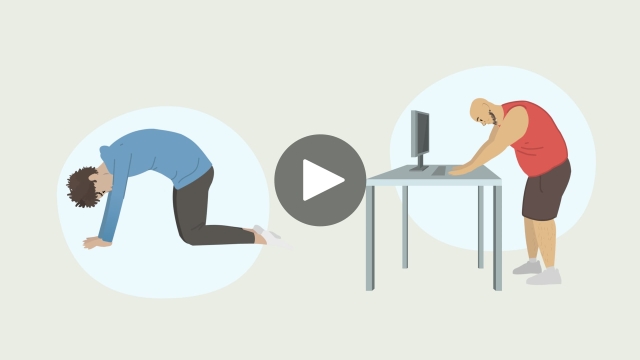
The following exercises can help you release and lengthen your pelvic floor muscles. This can support bladder and bowel health and reduce discomfort.
It's best to consult a pelvic health therapist before starting a new exercise routine to manage pelvic floor concerns, though the below exercises are some safe steps you can take at home to help you get started. They can also be helpful in preparing for surgery. If you’ve recently had surgery, talk to your surgeon before starting these exercises.
You can do these exercises and stretches as often as you’d like, or incorporate them into an existing movement routine.
It’s okay if you don’t feel much movement at first—connecting with this part of your body can take time.
Tucking, shapewear, binding, and the pelvic floor
It can be helpful to practice breathing exercises such as diaphragmatic breathing before or after tucking Method of positioning the penis and testicles so as to conceal them. your genitals, wearing shapewear or wearing a binder.